What is Guided Tissue Regeneration (GTR)?, An Overview
Guided Tissue Regeneration (GTR) is a surgical procedure designed to regenerate lost bone and tissues due to periodontal disease, utilizing barriers to facilitate healing․
GTR leverages the body’s natural regenerative capabilities, specifically focusing on rebuilding tissues damaged by gum disease, offering a targeted approach to periodontal restoration․
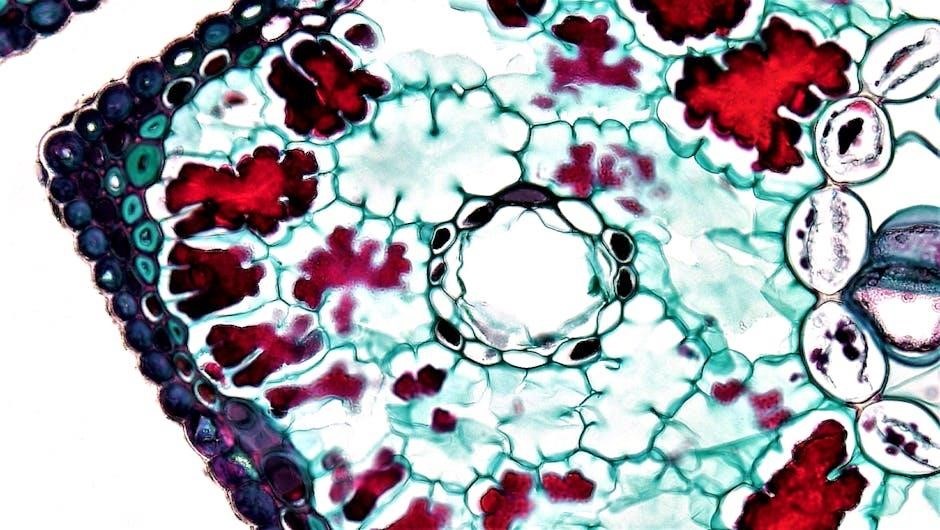
Periodontal regeneration represents a paradigm shift in treating gum disease, moving beyond simply managing the symptoms to actively restoring lost tissues․ Traditionally, periodontal surgery focused on removing infected tissue and reshaping gums․ However, Guided Tissue Regeneration (GTR) introduces the concept of rebuilding the supporting structures of teeth – the bone and ligaments – lost due to periodontal disease․
This innovative approach acknowledges the body’s inherent capacity for regeneration, but recognizes that it often requires guidance to occur effectively․ GTR aims to create a protected environment where bone-producing cells can thrive, while preventing the faster-growing soft tissues from interfering with this process․ It’s a biological approach, harnessing the body’s own healing mechanisms for long-term stability and improved periodontal health․
The Core Principle of GTR
The fundamental principle of Guided Tissue Regeneration (GTR) centers around selectively excluding epithelial and connective tissue cells from entering the periodontal defect․ This is achieved using a physical barrier – a membrane – that acts as a temporary blockade․ This barrier prevents the rapid migration of soft tissues, which would otherwise hinder bone and ligament regeneration․
By creating a protected space, GTR allows the slower-moving bone-producing cells to populate the defect and rebuild the lost support structures․ Essentially, it’s about directing the natural healing process, guiding it towards bone formation rather than soft tissue overgrowth․ This selective barrier is crucial for successful periodontal regeneration, fostering long-term stability․

How Guided Tissue Regeneration Works
GTR works by utilizing a membrane to physically separate the gum tissue from the bone, creating a space for bone-producing cells to regenerate lost support structures․
The Role of the Membrane Barrier
The membrane barrier is central to the GTR process, acting as a selective filter during healing․ It’s designed to prevent the rapid migration of epithelial and connective tissue cells into the bony defect․ This exclusion is vital, as these soft tissues would hinder bone regeneration․
Instead, the membrane allows the slower-moving bone-producing cells – osteoblasts – to populate the defect area and rebuild lost bone and periodontal ligament attachment․ Both resorbable and non-resorbable membranes are utilized, each offering distinct advantages depending on the clinical situation․
Essentially, the barrier guides the regenerative process, ensuring bone, rather than gum tissue, fills the space, restoring proper periodontal support․
Blocking Soft Tissue Ingrowth
A key principle of GTR is physically blocking the ingress of soft tissue cells into the periodontal defect․ Epithelial and connective tissue cells migrate much faster than bone-forming cells․ Without a barrier, these faster-growing tissues would colonize the defect, preventing bone regeneration and hindering attachment․
The membrane acts as a physical barrier, preventing this unwanted soft tissue in-growth․ This creates a protected space where bone cells can migrate and proliferate undisturbed․ This selective exclusion is crucial for successful regeneration, allowing the desired hard tissue response to dominate the healing process․
Effectively, the membrane ‘guides’ the healing, ensuring bone, not soft tissue, fills the defect․
Promoting Bone-Producing Cell Migration
Alongside blocking soft tissue, GTR membranes actively encourage the migration of bone-producing cells – specifically, osteoblasts and progenitor cells – into the defect site․ The membrane provides a scaffold and protected environment, facilitating their movement and differentiation․
These cells originate from the surrounding bone and periodontal ligament․ The barrier maintains space, allowing them to populate the defect and begin forming new cementum, periodontal ligament fibers, and alveolar bone․ This controlled access is vital for predictable bone regeneration․
Essentially, the membrane directs the body’s natural healing response towards bone formation, restoring lost periodontal support․

Types of GTR Membranes
GTR utilizes resorbable or non-resorbable membranes, acting as barriers to guide tissue regeneration․ These materials prevent soft tissue ingrowth, enabling bone cell migration․
Membrane choice depends on clinical needs and surgeon preference, impacting healing and post-operative protocols․
Resorbable Membranes: Advantages and Materials
Resorbable membranes offer significant advantages in GTR procedures, primarily simplifying the surgical process by eliminating the need for a second surgery to remove the membrane․ This translates to reduced patient discomfort and cost-effectiveness․ These membranes are designed to degrade naturally over time as the tissues heal, becoming integrated into the newly formed periodontal structures․
Common materials used in resorbable membranes include collagen, polylactic acid (PLA), polyglycolic acid (PGA), and combinations thereof․ Bioresorbable barrier materials, like Guidor AB, streamline the process into a single-step procedure․ The degradation rate is carefully controlled to coincide with the pace of tissue regeneration, ensuring optimal support during the critical healing phase․ This allows for a more predictable and less invasive treatment option for patients undergoing GTR․
Non-Resorbable Membranes: Characteristics and Use
Non-resorbable membranes, traditionally utilized in GTR, are composed of materials like expanded polytetrafluoroethylene (ePTFE) – commonly known as Gore-Tex․ These membranes maintain their structural integrity throughout the healing period, providing a stable barrier against soft tissue ingrowth․ A key characteristic is their requirement for surgical removal after the desired bone regeneration has occurred, necessitating a second surgical intervention․
While requiring an additional procedure, non-resorbable membranes offer predictable barrier function and are particularly useful in complex cases where prolonged protection is needed․ They effectively block the migration of epithelial and connective tissue cells, allowing bone-producing cells to populate the defect site․ Their robust nature ensures consistent performance during the regenerative process․

Clinical Applications of GTR
GTR effectively addresses infrabony defects and furcation involvement, offering a targeted solution for tissue regeneration in areas compromised by periodontal disease and bone loss․
Treatment of Infrabony Defects
Guided Tissue Regeneration (GTR) demonstrates significant efficacy in treating infrabony defects – those occurring below the crest of the bone – commonly caused by periodontal disease․ These defects often present challenges for traditional surgical approaches like open-flap debridement․
GTR utilizes membrane barriers to physically exclude the ingress of soft tissue cells, creating a protected space for bone-producing cells to migrate and regenerate lost bone․ This is particularly beneficial in deep, narrow defects (around 3mm depth) where bone regeneration is more predictable․

By promoting bone regrowth within the defect, GTR aims to restore lost periodontal support, reduce pocket depths, and improve clinical attachment levels, ultimately enhancing long-term tooth stability and function․
Addressing Furcation Involvement
Guided Tissue Regeneration (GTR) offers a valuable treatment modality for addressing furcation involvement, where periodontal disease has affected the area between tooth roots․ These complex defects pose a significant challenge to conventional surgical techniques․
GTR, in cases of mild to moderate furcation involvement, can effectively regenerate lost bone and attachment within the furcation area․ The membrane barrier prevents soft tissue from entering, allowing bone-producing cells to repopulate the space and rebuild support․
Successful GTR in furcations relies on meticulous surgical technique, thorough debridement, and stable wound closure․ It aims to arrest disease progression and potentially restore some function to the affected tooth․

Surgical Protocol for GTR

GTR surgery involves careful pre-surgical planning, precise membrane placement, thorough debridement, and meticulous wound closure to promote guided tissue regeneration and healing․
Pre-Surgical Assessment and Planning
Comprehensive evaluation is crucial before initiating GTR․ This begins with a detailed periodontal charting, meticulously documenting probing depths, clinical attachment levels, and furcation involvement․ Radiographic assessment, including bitewing and periapical views, is essential to visualize infrabony defects and assess bone levels․
Patient medical and dental histories are reviewed to identify any systemic factors that could impact healing, such as diabetes or smoking․ A thorough understanding of the defect morphology – depth and width – guides membrane selection and surgical approach․ Plaque control assessment is vital; patients must demonstrate commitment to rigorous oral hygiene․ Finally, soft tissue biotype evaluation helps predict healing outcomes and potential complications․
Surgical Procedure: Step-by-Step
The GTR surgical process begins with careful flap elevation to access the periodontal defect․ Thorough debridement removes infected tissue and creates a clean surface․ Next, the selected GTR membrane – resorbable or non-resorbable – is meticulously adapted to the defect, ensuring complete coverage of the bony defect․
The membrane is secured with sutures, creating a space to exclude soft tissue ingrowth․ Bone grafting materials may be added to enhance bone regeneration within the protected space․ Precise wound closure is achieved, ensuring primary intention healing and membrane stability․ Post-operative instructions emphasize gentle handling of the surgical site․
Wound Closure and Stabilization
Achieving meticulous wound closure is paramount in GTR success․ Sutures are carefully placed to ensure complete adaptation of the flaps and secure membrane positioning, preventing exposure․ Proper stabilization minimizes movement, crucial for undisturbed healing and preventing infection․
A periodontal dressing may be applied for added protection and comfort, further stabilizing the surgical site․ Patients receive detailed post-operative instructions emphasizing soft diet, gentle oral hygiene, and avoidance of trauma․ Regular follow-up appointments monitor healing, assess membrane integrity, and ensure optimal outcomes․

Factors Influencing GTR Success
GTR outcomes depend on diligent plaque control, defect shape (narrow and deep are ideal), robust soft tissue, surgical precision, and consistent post-operative care․
Importance of Plaque Control
Maintaining exceptional plaque control is paramount to the long-term success of Guided Tissue Regeneration (GTR)․ The regenerated tissues are susceptible to reinfection if bacterial biofilms are not meticulously managed․
Post-surgical, patients must adhere to a strict oral hygiene regimen, including frequent brushing, flossing, and potentially the use of antimicrobial mouth rinses․
Without diligent plaque removal, the inflammatory response can undermine the regenerative process, leading to pocket reformation and eventual failure of the GTR procedure․
Regular professional maintenance appointments are also crucial for sustained periodontal health following GTR treatment․
Defect Morphology (Depth and Width)
The characteristics of the bony defect significantly influence GTR outcomes․ Deep and narrow intrabony defects, ideally around 3mm in depth, generally exhibit higher success rates․
These configurations provide a more contained space for guided tissue regeneration, facilitating predictable bone fill․
Wider defects present a greater challenge, as soft tissue ingrowth can compromise the regenerative process․
Careful pre-surgical assessment, including radiographic evaluation, is essential to determine defect morphology and tailor the GTR approach accordingly, maximizing the potential for successful regeneration․
Soft Tissue Biotype Considerations
The patient’s soft tissue biotype – whether thick or thin – plays a crucial role in GTR success․ Thick soft tissue, approximately 1mm or greater, generally provides a more stable and predictable environment for regeneration․
It offers better vascularization and resistance to recession, enhancing wound stability․
Thin biotypes, conversely, are more prone to collapse and may require additional procedures, such as connective tissue grafting, to augment the tissue volume․
Careful evaluation of the soft tissue phenotype is therefore essential during treatment planning to optimize GTR outcomes․
Post-Operative Care and Healing
Post-operative success hinges on maintaining wound stability and diligent plaque control, alongside allowing an adequate healing period for tissue regeneration to occur effectively․
Maintaining Wound Stability
Ensuring wound stability post-GTR surgery is paramount for successful tissue regeneration․ This involves meticulous adherence to post-operative instructions provided by your dental professional․ Avoiding disruptive activities, such as strenuous exercise or probing the surgical site, is crucial during the initial healing phase․
A soft diet is typically recommended to minimize pressure on the treated area, preventing displacement of the membrane or disruption of the forming clot․ Patients are often advised to avoid brushing directly on the surgical site for a specified period, instead opting for gentle rinsing with prescribed mouthwash․
Regular follow-up appointments are essential to monitor healing progress and address any concerns promptly, contributing to optimal outcomes and long-term stability of the regenerated tissues․
Adequate Healing Period
Allowing for a sufficient healing period is a cornerstone of successful Guided Tissue Regeneration (GTR)․ The timeframe for complete regeneration varies depending on the extent of the defect and individual healing capacity, typically ranging from several weeks to months․
During this period, it’s vital to maintain impeccable oral hygiene, including gentle brushing and prescribed mouth rinses, to prevent infection and promote optimal tissue development․ Avoiding any actions that could compromise the surgical site, like smoking or consuming hard foods, is also essential․
Regular monitoring by your dentist through follow-up appointments ensures proper healing and allows for timely intervention if any complications arise, maximizing the long-term benefits of the GTR procedure․

Benefits of GTR Compared to Traditional Surgery
GTR offers superior clinical attachment levels (CAL) and reduced periodontal pocket depths (PD) compared to conventional open-flap debridement, especially for infrabony defects․
This regenerative approach provides more predictable and stable long-term results, fostering lasting periodontal health․
Improved Clinical Attachment Level (CAL)
Guided Tissue Regeneration (GTR) demonstrably enhances clinical attachment levels (CAL), a crucial indicator of periodontal health․ Traditional surgical methods, like scaling and root planing, often achieve attachment gain through long junctional epithelium formation, which is less stable․
GTR, however, promotes true periodontal tissue regeneration – the formation of new cementum, periodontal ligament, and alveolar bone – leading to a more robust and lasting CAL improvement․ This is achieved by physically blocking epithelial down-growth with a membrane, allowing connective tissue cells to attach directly to the root surface․
Consequently, patients undergoing GTR often experience a significant and measurable increase in CAL, contributing to improved tooth support and overall periodontal stability․ This represents a substantial benefit over conventional surgical approaches․
Reduction in Periodontal Pocket Depth (PD)
Guided Tissue Regeneration (GTR) effectively reduces periodontal pocket depth (PD), a primary goal in periodontal therapy․ Deep pockets harbor bacteria and contribute to ongoing inflammation and bone loss․ GTR addresses this by facilitating the regeneration of lost periodontal tissues, including alveolar bone and connective tissue attachment․
By creating a physical barrier, GTR prevents the formation of a pseudo-pocket – a reduction in PD achieved solely through soft tissue collapse․ Instead, it encourages genuine tissue regeneration, resulting in a lasting decrease in PD and improved access for oral hygiene;
This reduction in PD contributes to a healthier periodontal environment, minimizing bacterial accumulation and promoting long-term periodontal stability․
